27.10.2025
Colorectal Cancer: Comprehensive Overview, Prevention & Treatment
Table of Contents
1. Introduction: Why Colorectal Cancer Matters
2. What is Colorectal Cancer?
3. Causes & Risk Factors
4. Screening & Early Detection
5. Symptoms & When to See a Doctor
6. Diagnosis & Staging
7. Multidisciplinary Treatment Approaches
• Surgery & Locoregional Therapies
• Chemotherapy, Targeted Therapy & Immunotherapy
• Precision Medicine & Biomarkers
• Palliative & Supportive Care
8. Prevention & Lifestyle Modifications
9. Prognosis & Follow-Up
10. How RecMed Supports Patients
11. FAQs
12. References
1. Introduction: Why Colorectal Cancer Matters
Colorectal cancer (CRC) is among the most common malignancies worldwide and represents a substantial burden in morbidity and mortality. In the U.S. alone, an estimated 154,270 new cases of colorectal cancer are expected in 2025, with approximately 52,900 deaths. Early detection and a coordinated multidisciplinary approach are essential to improving outcomes.
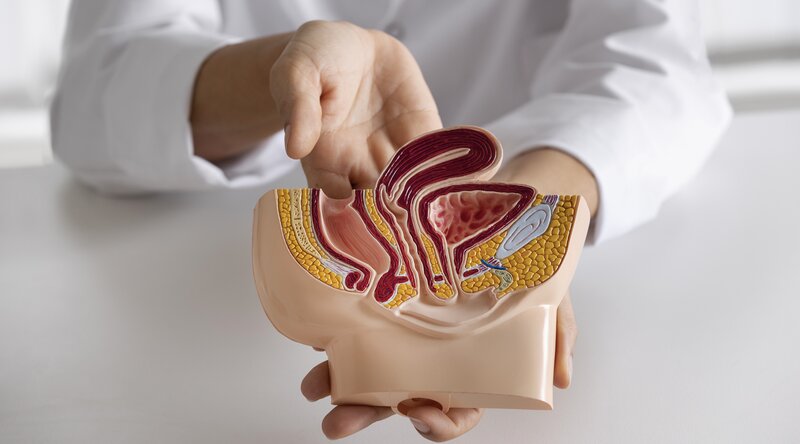
2. What is Colorectal Cancer?
Colorectal cancer refers to malignant growths arising in the colon or rectum. It encompasses colon cancer and rectal cancer. These tumours typically develop from adenomatous polyps over years and may spread (metastasize) to lymph nodes, liver, lungs, and other organs.
3. Causes & Risk Factors
Major risk factors include:
• Age (most cases diagnosed in individuals over age 50)
• Family history and inherited syndromes (e.g., Lynch syndrome, familial adenomatous polyposis)
• Lifestyle factors: diet high in red/processed meat, low in fibre, obesity, sedentary behaviour, smoking, heavy alcohol use
• Inflammatory bowel disease (ulcerative colitis, Crohn’s)
Understanding these allows for targeted screening and prevention strategies.
4. Screening & Early Detection
Screening is pivotal because early-stage colorectal cancer may be asymptomatic. Key screening methods:
• Colonoscopy (gold standard)
• Fecal immunochemical test (FIT) / stool DNA tests
• Flexible sigmoidoscopy
Delays in screening have been linked to worse outcomes.
Public health initiatives must emphasise screening uptake and risk-aware strategies.
5. Symptoms & When to See a Doctor
While early disease may not cause symptoms, signs to watch for include:
• A change in bowel habits (diarrhoea or constipation)
• Blood in stool or dark stool (melena)
• Abdominal discomfort, cramps, or bloating
• Unexplained weight loss or fatigue
• Iron-deficiency anaemia in older adults
If any of these occur, prompt medical evaluation is advised.
6. Diagnosis & Staging
Once suspicious signs appear, the diagnostic work-up includes:
• Colonoscopy with biopsy for histological confirmation
• Imaging (CT, MRI, PET) to assess extent and spread
• Laboratory tests (CEA tumour marker, liver function)
• Staging system (TNM, plus consideration for metastases)
The stage at diagnosis heavily influences management and prognosis.
7. Multidisciplinary Treatment Approaches
An optimal treatment plan involves a multidisciplinary team — including colorectal surgeon, medical oncologist, radiation oncologist, pathologist, radiologist, genetic counsellor, nutritionist, and palliative care specialist.
Surgery & Locoregional Therapies
For early-stage disease, surgical resection is often curative. In rectal cancer, surgery may be preceded or followed by radiotherapy/chemoradiotherapy.
In metastatic disease, metastasectomy or ablative therapies (e.g., liver metastasis ablation) may be used in selected cases.
Chemotherapy, Targeted Therapy & Immunotherapy
Standard chemotherapy remains a backbone in CRC treatment, especially for metastatic disease. Recent advances include targeted therapies (e.g., EGFR inhibitors, BRAF inhibitors) and immunotherapy for specific biomarker-positive tumours.
Precision Medicine & Biomarkers
Molecular profiling (e.g., RAS/RAF mutations, MSI status, HER2 amplification) allows tailoring of therapy and improves outcomes.
Emerging biomarkers and ctDNA may guide treatment decisions and monitoring.
Palliative & Supportive Care
From the outset, supportive care plays a role in symptom management (pain, bowel obstruction, metastatic complications), nutritional support, psychosocial care, and survivorship planning.
8. Prevention & Lifestyle Modifications
Prevention strategies include:
• Adopting a diet rich in fibre, fruits and vegetables
• Limiting red and processed meats
• Regular physical activity
• Maintaining a healthy weight
• Avoiding tobacco and limiting alcohol
• Participation in recommended screening programmes
Validating these measures in population studies supports their importance.
9. Prognosis & Follow-Up
Prognosis depends on stage, tumour biology, response to treatment, and comorbidities.
Follow-up care includes: periodic colonoscopy, imaging where appropriate, monitoring for recurrence, managing late effects of therapy, and lifestyle counselling.
10. How RecMed Supports Patients
At RecMed Medical Travel (Istanbul, Türkiye) we provide:
• Coordinated multidisciplinary care for colorectal cancer patients, including international referrals
• Access to advanced diagnostic techniques (molecular profiling, ctDNA testing)
• State-of-the-art surgical, locoregional, systemic treatments and supportive care
• Tailored travel, logistics, and translation services for global patients
Our goal: to deliver personalised, comprehensive care that aligns with the latest international guidelines and research.
11. FAQs
Is colorectal cancer preventable?
Yes—many cases are preventable with lifestyle changes and timely screening.
What is the role of molecular profiling?
It identifies actionable genetic mutations and helps personalise therapy.
Can metastatic colorectal cancer be cured?
Whilst cure is less likely in advanced disease, long-term control and survival are increasingly achievable with modern therapies.
12. References
1. SEER Cancer Stat Facts: Colorectal Cancer. U.S. National Cancer Institute.
2. American Cancer Society. How Common Is Colorectal Cancer?
3. Cornista AM, et al. Colorectal Cancer Immunotherapy: State of the Art and Future Directions.
4. Xie YH, et al. Comprehensive review of targeted therapy for colorectal cancer.
5. Pathak PS. State-of-the-Art Management of Colorectal Cancer.
6. “Current and emerging therapeutic approaches for colorectal cancer.” PMC.